
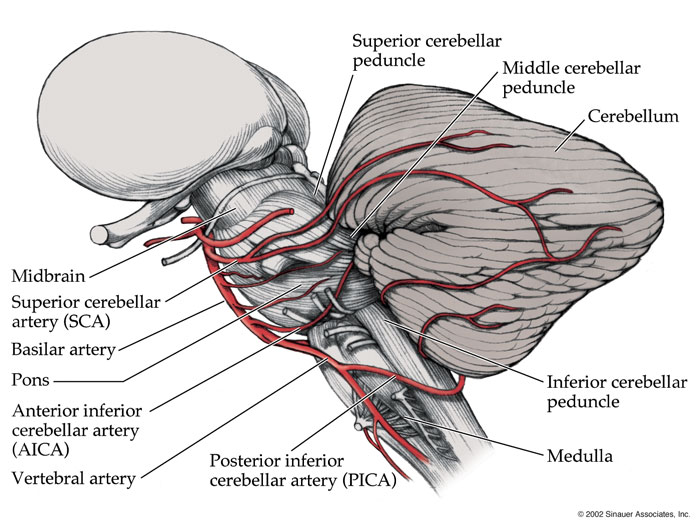
Susceptibility-weighted image (SWI) in a follow-up MRI showed a blooming effect around the c-PICA originating from the right vertebral artery. 2C) This flow variation in the c-PICA indicates arterial dissection rather than atherosclerosis. Approximately 3 months later, follow-up TOF-MRA re-visualized the c-PICA. 2B) There was no clinical or radiological progression of PICA infarction. 2A) Intriguingly, follow-up TOF-MRA on the 12th hospital day did not visualize the c-PICA, suggesting its flow disturbance. Eccentric enhancement of the c-PICA in 3D multi-planar reformatted (MPR) images supported atherosclerosis or arterial dissection rather than vasculitis. On the 3rd hospital day, we initiated mannitol application to prevent brainstem compression resulting from edematous change of the left cerebellar infarct.īecause she was young among patients with acute ischemic stroke and experienced sustained headache in the right occipital region, we were strongly suspicious of arterial dissection, particularly in the right vertebral artery or c-PICA. Follow-up computed tomography (CT) showed neither edema progression nor hemorrhagic transformation on the left cerebellar infarct. On the 2nd hospital day, she started to express sustained stabbing headache in the right temporo-occipital region with right facial hypesthesia and dysphagia on neurological examination. 1B) We immediately administered a standard regimen comprising intravenous hydration, antiplatelet loading and high dose statins. 1A) Time of flight-magnetic resonance angiography (TOF-MRA) showed the right PICA arising from right vertebral artery, but not the left PICA.

Diffusion-weighted MRI confirmed right lateral medullary infarct and left cerebellar infarct in bilateral PICA territories. Neurological examination revealed right ptosis, right upper and lower limb ataxia and gaze-evoked nystagmus, suggestive of Wallenberg’s syndrome. She also complained of gait imbalance and nausea. Key words: Cerebellar infarct Lateral medullary infarct Common PICA Arterial dissection High-resolution MRIĪ 57-year-old female patient visited the emergency room (ER) due to acute sustained vertigo which started about 20 hours before she arrived ER during travel in Shanghai. We investigated the mechanism and etiology of bilateral PICA territory infarcts using DSA and high-resolution magnetic resonance imaging (MRI) and elucidated the dissection of the c-PICA. Susceptibility-weighted image showed a blooming effect around the c-PICA and the phase map revealed eccentric high signal intensity on the vessel wall of the c-PICA, implicating intramural thrombus in c-PICA dissection. Eccentric enhancement of the c-PICA on 3D multi-planar reformatted images suggested arterial dissection or atherosclerosis rather than vasculitis. Digital subtraction angiography (DSA) revealed that bilateral PICAs originated from the c-PICA arising from the right vertebral artery with luminal irregularity. We report a case of bilateral PICA territory infarcts involving right lateral medulla and left cerebellum via spontaneous c-PICA dissection. Bilateral cerebellar infarcts in posterior inferior cerebellar artery (PICA) territories have been previously reported and the common PICA (c-PICA) on one side was proposed as a possible mechanism.


 0 kommentar(er)
0 kommentar(er)
